Angina is a tight or heavy chest pain that typically comes on during exertion or at times of stress. Angina happens when the heart muscle doesn’t get enough oxygen-rich blood for its needs.
It is commonly caused by coronary heart disease, where the arteries supplying the heart muscle become narrowed or blocked by a build-up of fatty deposits, or atherosclerosis.
Coronary heart disease (CHD) affects more than two million people in the UK. As well as causing angina, it can lead to heart attacks that can permanently damage your heart and result in premature death. The good news is that if your angina is identified early and treated effectively, you can protect your heart.
What is angina?
Angina is the name for pain or discomfort in the chest, usually caused by CHD. The British Heart Foundation describes angina as:
Angina is a symptom. It’s a pain or an uncomfortable feeling when blood flow to your heart is reduced. It’s not dangerous, but it can be a sign of heart problems, like coronary heart disease.
It’s usually felt in your chest. Some people feel pain in their arm, neck, stomach, back or jaw.
What is refractory angina?
Refractory angina is chest pain that isn’t controlled by the best available treatments.
There are many effective therapies for angina, including a range of medications, angioplasty to open up the blood vessels, and the insertion of stents, small tube-like structures, to hold open the coronary arteries and increase blood flow to the heart muscle. In more severe cases of CHD you may need heart bypass surgery.
You may have refractory angina if you still get angina symptoms despite having optimum treatment, including medical therapy, angioplasty or bypass surgery.
Indicators of refractory angina include:
- chronic angina-type chest pain for 3 months or more
- history of coronary artery disease
- pain associated with reversible ischaemia (lack of oxygen to the heart muscle) that remains after treatment
Refractory angina may happen if the narrowed coronary arteries are too small for stents, which can occur in diabetes, which damages small blood vessels in the heart.
Refractory angina causes pain, restricts your ability to exercise and perform daily activities and reduces your quality of life. It can cause anxiety, depression and repeated hospitalisations.
Angina symptoms
The main symptom of angina is chest pain or discomfort. You may notice chest tightness or a dull ache when exerting yourself during exercise, walking upstairs, or feeling stressed.
The pain may spread from your chest into your arm, jaw or neck or go through to your back. You may also notice:
- breathlessness
- feeling weak and faint
- nausea
- tiredness
- sweating
Angina usually stops when you rest. If the chest pain doesn’t go away, is more severe, or comes on when you’re resting, you may need urgent treatment to prevent or treat a heart attack.
What causes angina?
Angina is usually caused by coronary heart disease, the most common type of heart and circulatory disease.
In coronary heart disease, the blood vessels that supply blood to the heart are progressively narrowed by fatty plaques. The fatty deposits build up within the walls of the arteries, which narrows them and restricts blood flow to the heart muscles. This furring up of the vessels is known as atherosclerosis.
Blood supplies the food and oxygen the heart muscles need to work and stay alive. If the blood flow is restricted by atherosclerosis, the muscles don’t get enough oxygen which causes the chest pain in angina.
If a piece of the fatty material breaks off, a blood clot may form. This clot can block one of the coronary arteries, cutting off the supply of essential blood and oxygen. Without prompt medical treatment, cells in the heart muscle can die. This is known as a heart attack or myocardial infarction.
For more information, please read our article on ‘what is coronary heart disease?’
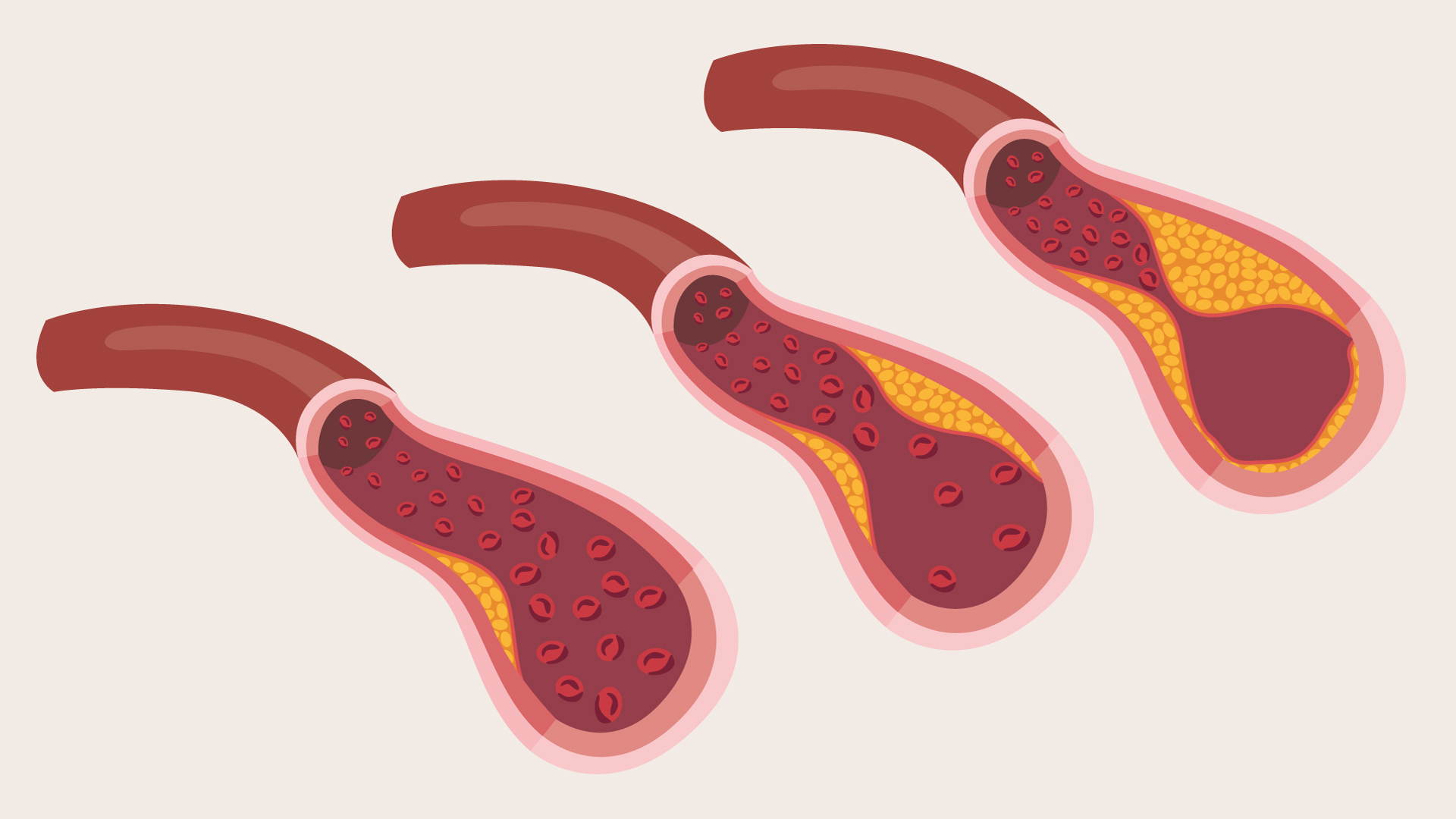
Angina is most commonly caused by coronary heart disease, the narrowing of the blood vessels (coronary arteries) that supply blood to the heart.
Who is at risk of angina?
Coronary heart disease is a common condition; there are 2.3 million people in the UK living with CHD, so anyone could potentially develop angina. However, some people are more at risk of getting angina.
Risk factors include:
- age, it is more common in the elderly
- male: coronary heart disease affects men more frequently as well as women after menopause
- hypertension
- family history of heart disease
- ethnicity: angina is more common in people with black African, African Caribbean and South Asian heritage
- high cholesterol, especially raised levels of LDL (also known as ‘bad’) cholesterol
- diabetes
- smoking
- being obese or overweight
- physical inactivity and not exercising regularly
Diagnosing angina
We have a rapid access cardiac clinic for patients experiencing chest pain.
If you have angina, your cardiologist may arrange investigations to diagnose coronary heart disease, check for other chronic conditions, and look at blood flow through the coronary arteries.
Diagnostic tests may include:
- an assessment of your lifestyle, medical history and family history
- blood pressure test
- blood tests, including a test to evaluate cholesterol and lipid levels in your blood
- chest x-ray
- electrocardiogram (ECG)
- ambulatory ECG recorders
- stress ECG test
- coronary CT angiography
- coronary angiography
- echocardiography and stress echo tests
Angina treatment
Angina treatment can increase the blood flow through the coronary arteries, reduce chest pain and prevent heart damage.
Your cardiologist will work with you to reduce your risk factors, control other medical conditions like hypertension and diabetes, and start treatments to boost blood flow to the heart muscles.
Treatments include:
- lifestyle changes
- medication
- coronary angioplasty and stenting
- coronary artery bypass graft
- coronary sinus reduction
Lifestyle changes
Making changes to your lifestyle can prevent coronary heart disease and stop your angina from getting worse. You can protect your heart by:
- stopping smoking
- exercising regularly
- losing weight to achieve a healthy BMI if you are overweight or obese
- eating a healthy, balanced diet and cutting back on salt and saturated fats
- taking medication to control any medical conditions like hypertension, high cholesterol and diabetes
Angina medication
- Nitrates open up the blood vessels and treat angina. Tablets or aerosol sprays under the tongue act rapidly to relieve pain. Tablets or self-adhesive patches release medicine over time to prevent angina
- Antiplatelet drugs such as aspirin, clopidogrel and ticagrelor make the blood less sticky
- Statins or PCSK9 inhibitors to reduce cholesterol
- ACE inhibitors treat hypertension and relax the blood vessels to increase blood flow
- Calcium channel blockers open up the coronary arteries and reduce blood pressure
- Beta-blockers treat hypertension, slow the heart rate and improve blood flow in the vessels
- Diuretics reduce excess fluid
Coronary angioplasty and stenting
Coronary angioplasty is a minimally invasive procedure that relieves coronary artery blockages and increases blood flow through the coronary arteries.
A specialist inserts a fine tube called a balloon catheter through a vessel in the groin into the blocked coronary artery.
They inflate the balloon within the narrowed artery, which stretches it open. Usually, they will then insert a small tube, called a stent, which stays in permanently to keep the vessel open.
Coronary artery bypass graft
If the coronary arteries are significantly narrowed, and angioplasty isn’t possible or has failed, surgery can bypass the blocked blood vessels.
In coronary artery bypass grafting or CABG, a cardiothoracic surgeon places a new blood vessel into the heart, stitching it to the existing arteries. The new blood vessel bypasses the narrowed artery, letting blood flow to the heart muscle.
Coronary sinus reduction
Coronary sinus reduction is an innovative minimally invasive procedure to treat refractory angina. The cardiologist introduces a small device called a reducer to narrow the coronary sinus and reduce blood flow through the channel.
The reducer increases the pressure in the sinus, increasing blood flow in the cardiac muscle and easing angina.
Locations
Treatment for angina is available in the following locations:
Discover our team of cardiology experts
Meet our team of leading cardiologists. From heart health to advanced interventions, our specialists are here to provide you with personalised care.
