Sarcoidosis is caused by the growth of tiny collections of inflammatory cells called granulomas. Sarcoidosis can affect any body area, but most commonly the lungs and lymph nodes. However, when these clusters of inflammatory cells impact the heart, it is known as cardiac sarcoidosis.
Cardiac sarcoidosis is rare and affects just 1 in every 10,000 people in the UK. Although no cure exists, treatments can improve your outlook and quality of life.
What is cardiac sarcoidosis?
Cardiac sarcoidosis is a rare type of heart condition believed to be caused by problems with your immune system.
The growth of areas of inflammatory white blood cells and other tissues, known as granulomas, characterises the disease. They can occur on the skin and inside the body, affecting the lungs and lymph nodes most often.
While these granulomas aren’t cancerous, they could cause serious health complications. This potential is especially true in cardiac sarcoidosis where granulomas form on the heart.
Unfortunately, cardiac sarcoidosis has a poor prognosis generally. However, treatments can help slow its progress and prolong your wellbeing.
Cardiac sarcoidosis symptoms
Depending on where it occurs in the body, sarcoidosis is often challenging to detect and diagnose until it is relatively advanced. This is why we sometimes call cardiac sarcoidosis a ‘silent killer’.
However, cardiac sarcoidosis causes various symptoms, including:
- irregular heartbeat
- dizziness
- fainting spells
- chest pain
- shortness of breath
Two symptoms can occur in the later stages of cardiac sarcoidosis — swelling of the legs and paroxysmal nocturnal dyspnea (on-and-off shortness of breath that wakes you at night).
However, these symptoms also apply to a range of other heart conditions, including a heart attack. So, you must schedule a consultation with a cardiac specialist to discuss your experiences and get a definitive diagnosis.
What causes cardiac sarcoidois?
We don’t know what causes cardiac sarcoidosis, however, researchers suggest that it is a result of an overactive response from your immune system to infectious or environmental substances, including allergens like pollen or dust, causing it to overproduce cells.
Some studies suggest that if a close blood relative has cardiac sarcoidosis, you are up to five times more likely to develop it.
People of African-Caribbean and Scandinavian origin are also more likely to develop sarcoidosis and it’s more common in women than men.
Sarcoidosis can affect people of any age, but usually appears in adults between 30 and 40 years old. It is rare in children.
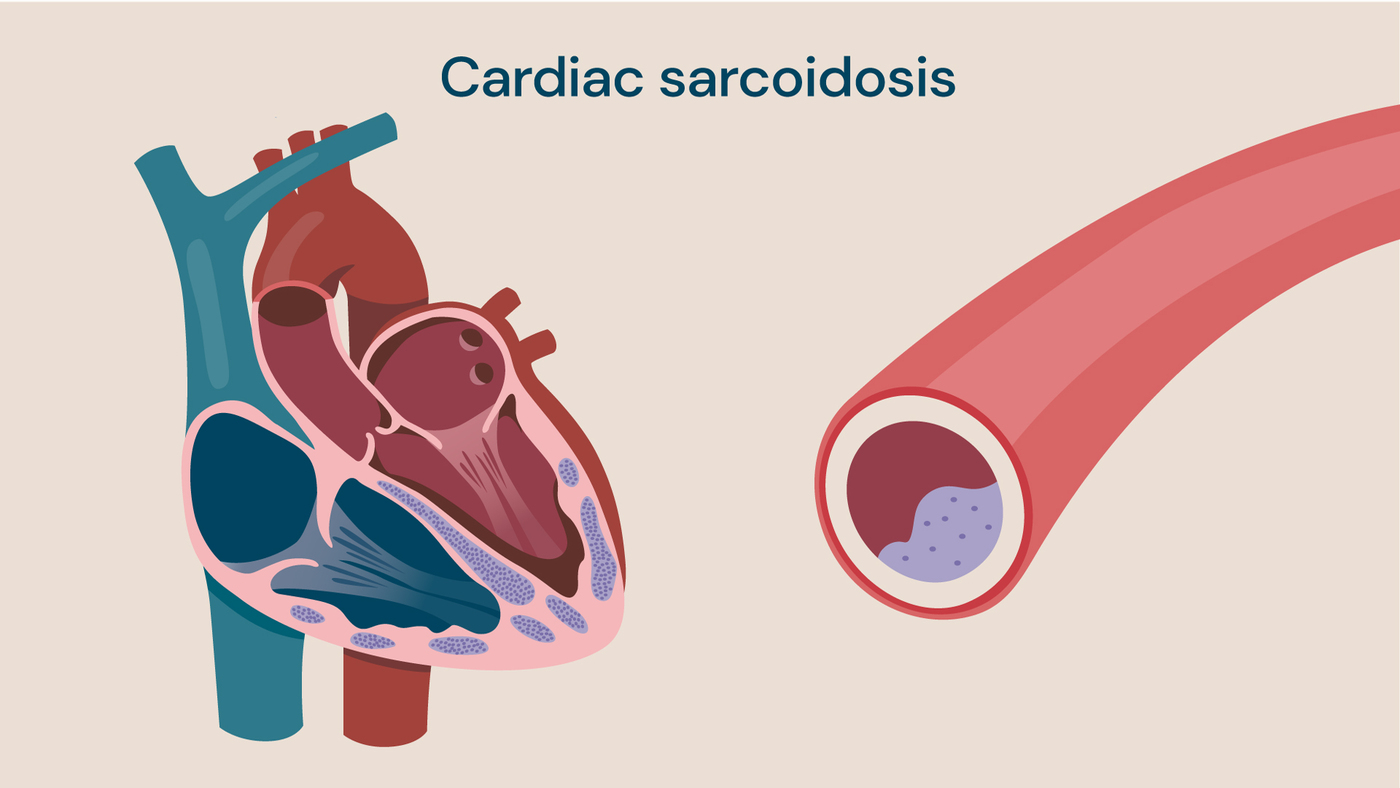
Granulomas can build up in the heart muscle leading to weakened heart beats and abnormal heart rhythms.
Risk factors of cardiac sarcoidosis
Cardiac sarcoidosis can affect any part of the heart muscle; the symptoms you experience will depend on the area. However, the condition can cause complications, including but not limited to:
- heart arrhythmia
- heart failure
- sudden cardiac arrest
Your risk of a severe cardiac event is higher if your heart’s left ventricle doesn’t pump blood as well as it should.
Diagnosing cardiac sarcoidosis
Cardiac sarcoidosis can be complicated for consultants to diagnose. They will need to understand your medical history and symptoms and give you a physical examination.
In addition, they may arrange for you to take a series of tests to confirm a diagnosis. These tests could include:
- electrocardiogram (ECG) – monitors the electrical activity inside your heart
- echocardiogram – an ultrasound test looking at your heart’s shape, size, overall appearance and function
- cardiac MRI – magnetic resonance imaging uses magnetic and radio waves to show detailed images of inside your heart
- PET scan – PET stands for positron emission tomography. It’s a scan that produces a 3D image of inside your body and can show how your heart is working
- cardiac biopsy – a cardiologist removes a small piece of the heart muscle and looks at it under a microscope. They use a small, thin tube called a catheter and insert it through a vein or artery near the heart
Timely diagnosis and treatment of cardiac sarcoidosis is important. Fortunately, our team of specialists use a combination of cardiology and respiratory expertise, allowing the design of a precise treatment strategy for each patient and the prevention of life-threatening complications.
Cardiac sarcoidosis treatment
Cardiac sarcoidosis has no cure, but various treatments can help control your condition. The type of treatment will depend on the disease’s severity and potentially how well you have responded to previous treatments for the disorder.
Common treatments for cardiac sarcoidosis include:
Corticosteroid medications
Often known as steroids, these medicines limit inflammation, stopping the growth of new granulomas and keeping your current level of disease stable. A common corticosteroid drug is prednisone.
Immunosuppressants
Several drugs can keep your immune system under control and prevent it from overreacting and causing new areas of inflammation.
Heartbeat regulation medications
If you are experiencing arrhythmia (irregular heartbeat) because of cardiac sarcoidosis, your consultant may prescribe medications to treat it.
Pacemaker
A pacemaker is a small electrical device fitted to your chest or abdomen to treat abnormal heart rhythms.
A pacemaker is a small electrical device fitted to your chest or abdomen to treat abnormal heart rhythms.
Implantable cardioverter defibrillator (ICD)
The ICD is a small, battery-powered device that a cardiologist or surgeon places in your chest. It continuously checks your heartbeat and delivers an electric shock when it needs to restore a regular heart rhythm.
Heart transplant
If your condition is so severe that it causes heart failure, you may be considered for a heart transplant.
Locations
Treatment for cardiac sarcoidosis is available at the following locations:
Discover our cardiac sarcoidosis experts
Check out our team of cardiologists specialising in cardiac sarcoidosis. Whether it’s managing heart health or delving into advanced interventions, our experts are geared up to offer tailored care just for you.
