What is transcatheter aortic valve implantation?
TAVI is a minimally invasive procedure in which a cardiothoracic surgeon inserts a new aortic valve into your heart to treat aortic stenosis. TAVI stands for transcatheter aortic valve implantation; it is sometimes known as TAVR, which stands for transcatheter aortic valve replacement.
TAVI is an alternative to open-heart valve replacement. Your specialist may recommend TAVI if traditional valve replacement surgery may be risky because of your age, health and wellbeing.
What to expect during TAVI
When you are referred for a TAVI, our MDT (multidisciplinary team) will carefully evaluate your case and advise on the best strategy to suit your anatomy in a more personalised way. Our operators are extremely experienced in all procedures for the aortic valve and will be able to offer an unbiased opinion based on the current best available scientific evidence.
Once the strategy has been agreed, the intervention on the heart will be performed to the highest standards in state-of-the-art facilities.
Your specialist will usually perform TAVI under local anaesthetic in the cardiac catheter laboratory or ‘cath lab’. However, general anaesthetics are available if that’s better for your needs.
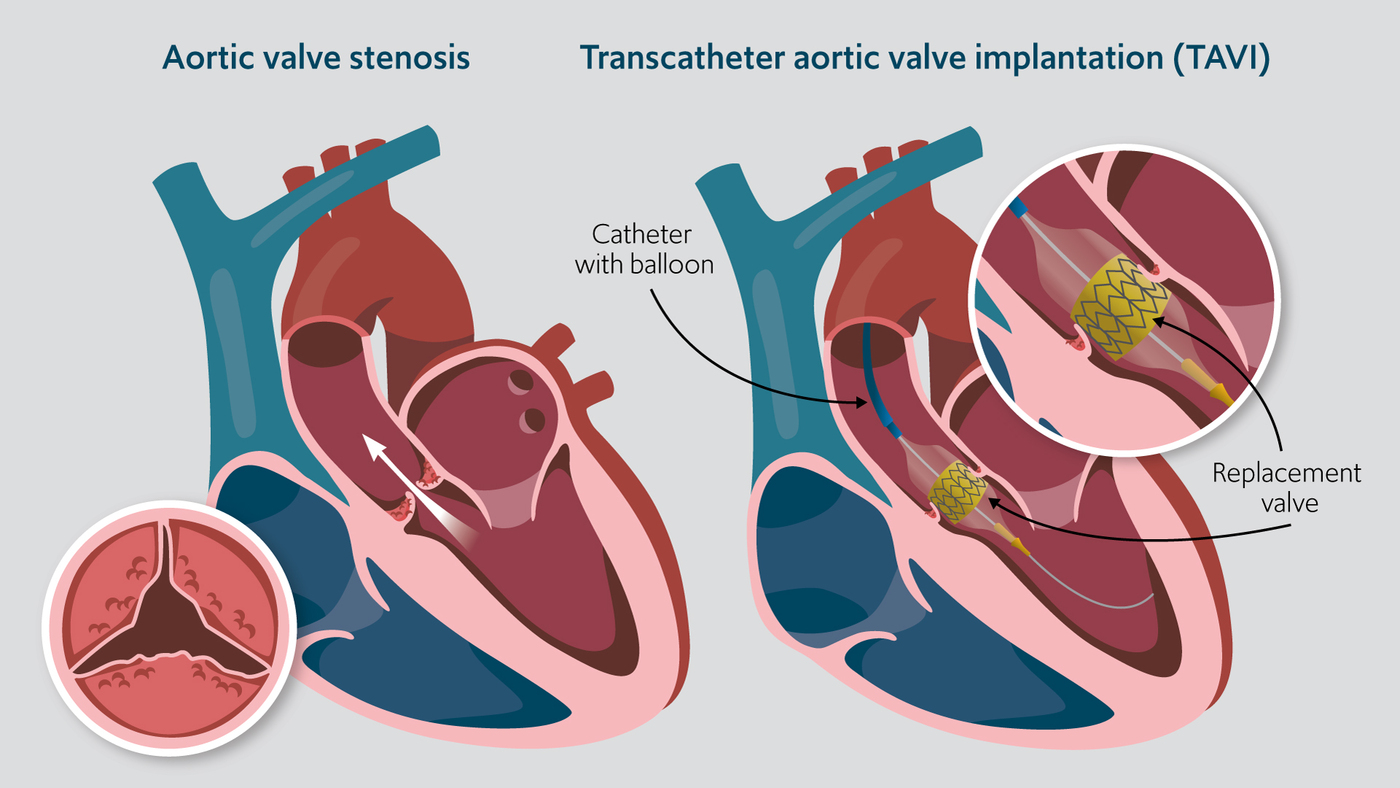
The doctor will make a small cut over blood vessels, usually in your groin or shoulder. They will insert fine flexible tubes called catheters into the artery and vein at the site. These allow your doctor to give any necessary drugs safely, access the heart to implant the valve, and fit a temporary pacemaker if they need to stabilise your heart’s rhythm.
The specialist places your new valve into the catheter. It is made of animal tissue, either porcine from pigs or bovine from cows. Using X-ray video guidance, they carefully guide the catheter through the artery to your heart. When the tip of the catheter reaches the damaged or diseased aortic valve, they implant the new valve.
Depending on the type of valve chosen, it will either expand spontaneously, or the consultant will use a balloon to open the valve. The prosthetic device flattens and pushes the damaged valve out of the way and takes over its function. They will stitch the valve to a mesh metal tube, called a stent.
Finally, the consultant will check that the new aortic valve is working, withdraw the catheter and close the incision. Both the valve and the stent will remain in your heart for the rest of your life.
How to prepare for TAV
TAVI treats a faulty aortic valve in adults with symptomatic aortic stenosis. It is occasionally used for carefully selected patients with aortic regurgitation. TAVI reduces distressing aortic stenosis symptoms, improves life expectancy and boosts the quality of life.
As a less invasive procedure, it is typically used for adults who are too frail and unwell for open-heart valve replacement surgery. The National Institute for Health and Care Excellence (NICE) only recommends TAVI for people unsuitable for surgical aortic valve replacement, but they are reviewing the guidance. They will decide whether to recommend TAVI for people who are only at intermediate or low risk for cardiac surgery for aortic valve disease because of the benefits of TAVI, including the local anaesthetic, minimally invasive procedure and shorter hospital stays.
What is aortic stenosis?
Aortic stenosis is a common heart condition where the aortic valve is stiff and narrowed. Calcium deposits make the flaps of tissue thicken and stiffen. The aortic valve can’t open properly and narrows, restricting blood flow.
Aortic stenosis makes it difficult for the heart to pump blood out of the heart and around the body. You may feel weak and tired and experience palpitations, chest pain and breathlessness, especially during exertion.
Aortic stenosis is progressive and, without treatment, will get worse over time. The heart has to work harder to pump blood through the narrowed valve, which can cause heart failure and dangerous arrhythmias. TAVI can ease symptoms and reduce the risk of complications, including heart failure and sudden death in the future.
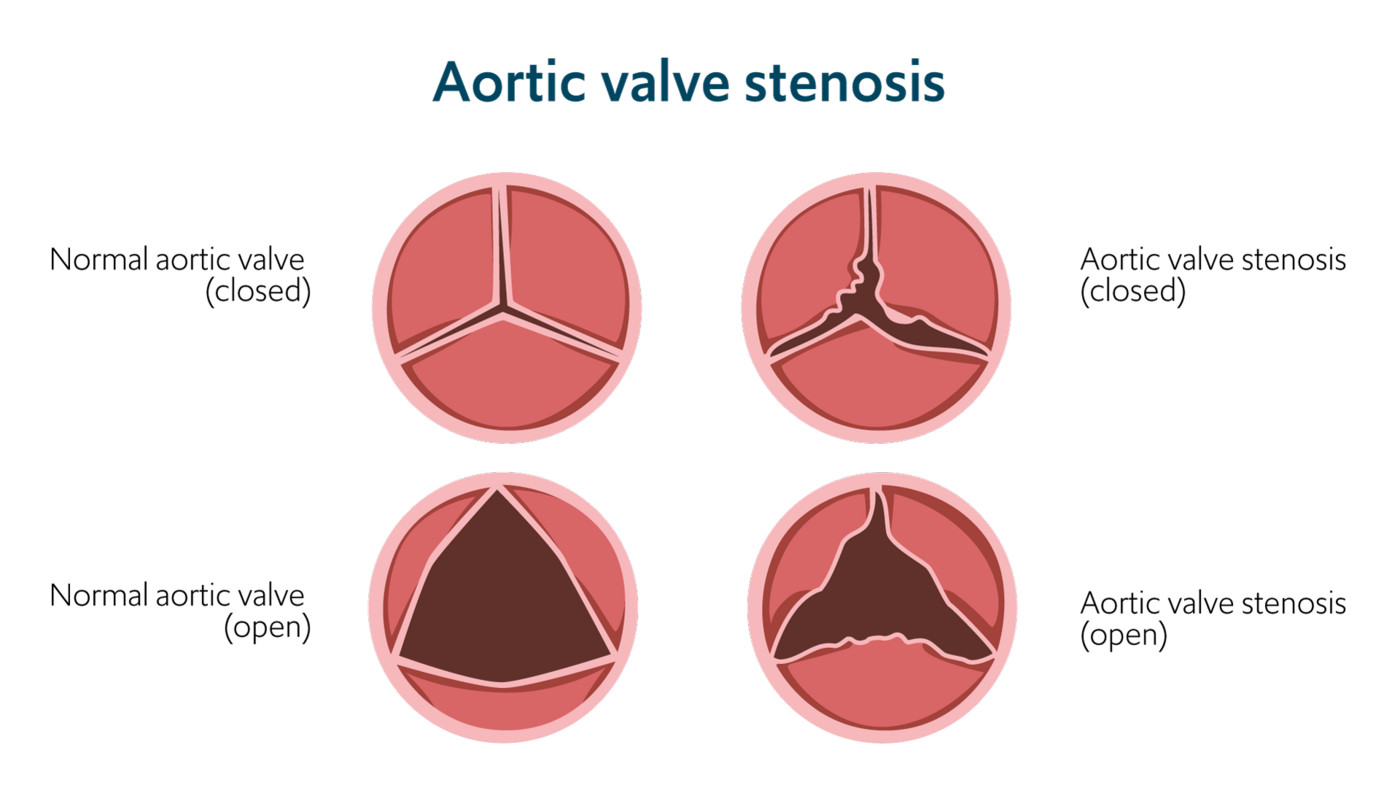
Aortic valve stenosis causes the valve to become narrowed, reducing blood flow through the heart.
How to prepare for TAVI
Before the procedure, your cardiology team will arrange investigations to confirm your diagnosis, assess the severity of your aortic stenosis and check your general health. They should discuss the results with you and decide whether TAVI is the best treatment for your needs. Investigations could include:
- blood tests
- ECG
- chest X-ray
- echocardiogram
- angiography
- cardiac MRI scan
- CT scan
- lung function tests
- exercise stress tests
Before your procedure, you should try to improve your health and prevent complications. It can help to:
- stop smoking to reduce breathing problems and improve healing
- aim to reach a healthy BMI if you are overweight; it will reduce the risk of the procedure
- have a dental check-up – tooth and gum disease can allow bacteria to enter the bloodstream and infect your new valve, a dangerous condition known as endocarditis
- see your GP to ensure any chronic medical problems like hypertension, bronchitis, and diabetes are well controlled
- to protect against infection, shower carefully the evening before and the morning of your TAVI. Pay careful attention to the skin creases in the armpits, groin, genitals and under your breasts
Recovery from TAVI
After your TAVI, the staff will monitor and support you in the recovery unit. You will have a drip for fluids and antibiotics, as well as a monitor to show your heart’s rate and rhythm. When you are stable, they will transfer you to the ward.
You will have a dressing over the wound and may notice some pain and bruising at the insertion site. This should get better over the first few days. The team will give you painkillers and ensure you’re comfortable.
Most people can go home three to five days after TAVI. Your team will arrange a follow-up appointment and an echocardiogram to check that the valve is working well.
If you feel unwell or have any concerns, contact the hospital, your GP or go to the nearest accident and emergency department.
Benefits of TAVI
All medical procedures have risks. Your team will work to reduce any complications and support your healthy recovery.
The risk of complications with TAVI depends on your general health and the health of your heart. People who have existing medical conditions may be more vulnerable to problems. Talk to your consultant about the risks and benefits of TAVI in your case.
Potential complications include:
- bleeding, bruising or infection at the access site
- one in 20 people will have damage to an artery that needs repair
- slow or irregular heart rate. 10-20% of people will need a permanent pacemaker to correct this
- heart attack affects less than one in a hundred people (0.7%). The doctor will usually open up the blocked blood vessel with angioplasty and insert a stent
- allergy to the dye during angiography
- if you develop complications during surgery, you may need open-heart surgery. This happens to under one in a hundred patients
- stroke – around 3% of people having TAVI have a stroke
- acute kidney failure, which is more common in people with impaired kidney function
- sadly, complications following TAVI may lead to death. Between 1% and 4% of people will die within 30 days of the procedure
Locations
Explore our team of cardiology specialists
Meet our team of renowned cardiac surgery specialists. From cardiovascular health assessments to innovative interventions, our experts are committed to delivering personalised care designed just for you.
