Targeted lung denervation: 90 minute treatment to improve lung function in COPD patients
Our consultants have worked with US-based company Nuvaira® to develop a novel device to treat patients with chronic obstructive pulmonary disease (COPD). The treatment has been found to significantly reduce instances of flare-ups and therefore reduce cases of hospitalisation in individuals with COPD, treating the cause of the condition, rather than only the symptoms.
What is COPD?
COPD is an umbrella term which covers a group of lung conditions that cause breathing difficulties. Common symptoms include breathlessness, cough, chest tightness, wheezing and excess mucus production (phlegm). When symptoms become severe, it is known as a COPD exacerbation, or flare up.
The most common lung conditions contributing to COPD are emphysema and chronic bronchitis, and they usually occur together. These conditions are typically caused by long-term exposure to particulate matter, such as that found in cigarette smoke.
Chronic bronchitis is inflammation of the bronchial tubes which carry air to and from air sacs called alveoli, which help pass oxygen to your blood. The condition is characterised by a daily cough and over production of mucus.
Emphysema is where the alveoli in the lungs become damaged, reducing their surface area and, in turn, reducing the amount of oxygen entering the blood stream.
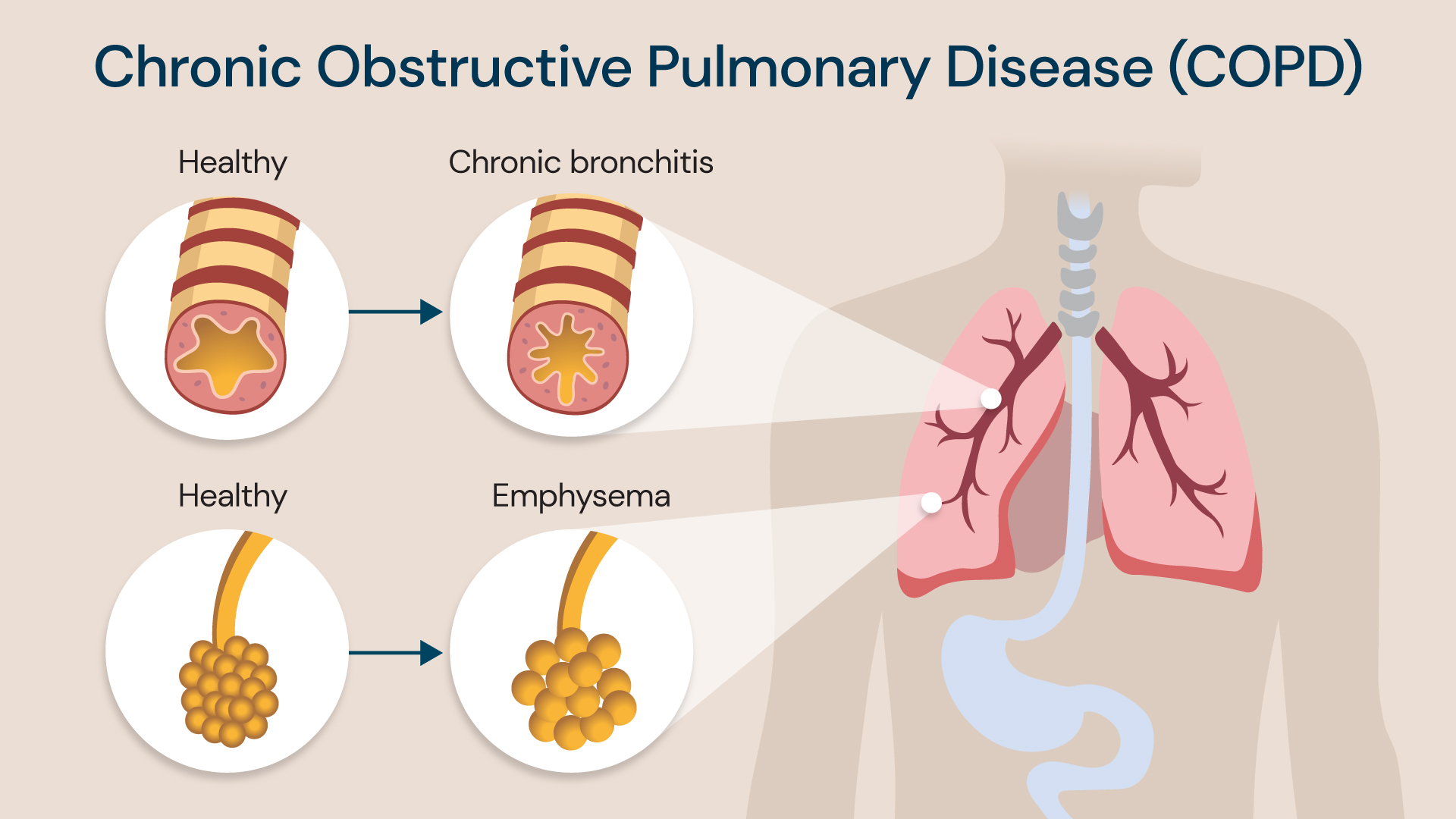
There are two types of COPD, chronic bronchitis and emphysema, which affect different parts of the lungs
The role of the vagus nerve in COPD
Common to all COPD patients is an overactive vagus nerve which branches into and controls various functions of the lungs. It stimulates the smooth muscles lining the bronchial tubes, causing them to constrict. The nerve also stimulates mucus production.
When the vagus nerve is overactive in the lungs, the airways become constricted and filled with too much mucus. This contributes to the symptoms experienced with COPD exacerbations.
Some of the medicines used in inhalers to treat COPD (called anticholinergic drugs) focus on reducing the sensitivity of smooth muscles lining the bronchial tubes to vagus nerve stimulation. This relaxes the airways to help patients breathe, as well as reducing symptoms like coughing.
However, these medicines do not treat the underlying problem of an overactive vagus nerve and so their effect is temporary.
Minimally invasive treatment for COPD
We now have a new minimally invasive long-term treatment for COPD designed to improve breathing and reduce the frequency of exacerbations in affected individuals.
Our consultants, Professor Pallav Shah, consultant physician in respiratory medicine, and Dr Justin Garner, consultant respiratory physician, worked with US-based company Nuvaira® to develop a new device and treatment for COPD, which we are proud to offer in the UK exclusively at Royal Brompton and Harefield hospitals.
Nuvaira’s dNerva lung denervation system is carried out under general anaesthetic, using an electrode to disrupt communication between the vagus nerve in the lungs and the brain.
Targeted lung denervation blocks the actions of the vagus nerve, and this has been found to lead to reduced symptoms and COPD exacerbations, and improved lung function and quality of life.
The treatment is thought to have long-term benefits and works synergistically with anticholinergic drugs which COPD patients rely on now.
Professor Shah explains, “treating the nerves in this way blocks their actions more efficiently than anticholinergic inhalers, which only work temporarily, can have an irregular distribution within the lungs and may cause side-effects such as blurred vision and urine retention in a small number of patients.
“This procedure keeps obstructed airways open to improve breathing and has the potential to provide a long-term improvement for all patients with COPD.”
Using this new device, Professor Shah has carried out more targeted lung denervation procedures than any other specialist globally, and we are delighted that our patients will benefit from the team’s vast experience in this area.
How does targeted lung denervation work?
“It works by inserting a camera into the lungs,” summarises Dr Garner. “A bronchoscope – a fibre optic cable with a camera on the end – is passed through the mouth and down into the lungs before a catheter is passed through the bronchoscope. The catheter has a balloon and an electrode on the end, and this is what we use to deliver the treatment.”
Once activated, the electrode delivers radiofrequency energy to the airways, penetrating the wall of the airways and interrupting the vagus nerves located just outside of the airways. This interruption prevents the brain signals to the lung from triggering a COPD exacerbation.
Once the radiofrequency energy has been delivered in one position, the balloon is deflated and rotated to the next position. This is repeated four times to treat each point of the airway’s circumference.
Both lungs are treated in the same session so after this process has been carried out on the first lung, it is repeated for the second lung. The procedure typically lasts for around 90 minutes before the catheter is then removed and the patient can begin their recovery process.
Nuvaira®’s trials over the last nine years have shown very promising results. “We’ve seen significant improvements, particularly in exacerbation frequency,” says Professor Shah, “which translates into reduced admissions to hospital and a better quality of life.”
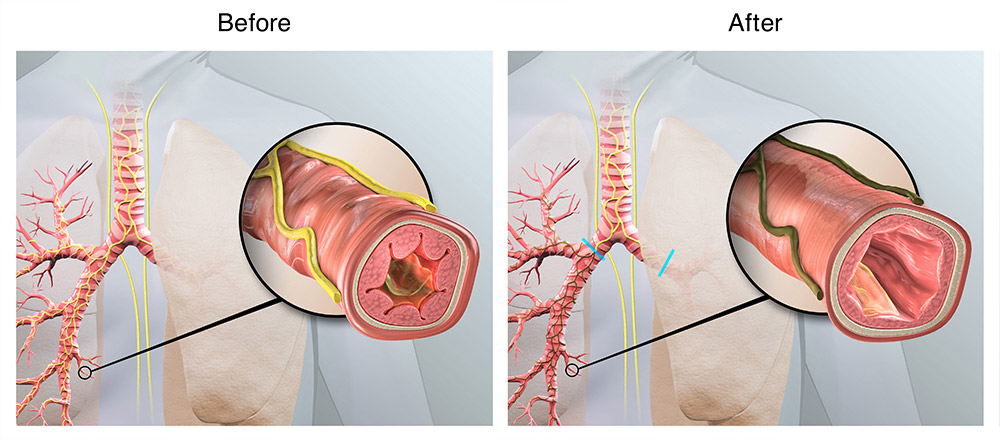
Airway before and after targeted lung denervation, with less mucus and swelling shown after the Nuvaira® Lung Denervation System
Life after targeted lung denervation treatment
Patients usually spend two hours in the recovery lounge following their procedure, before going home. After a few days, they usually feel well enough to return to work and other daily activities.
Following the treatment, the signals or impulses from the brain do not reach the lungs, preventing the excess production of mucus. There is also relaxation of the bronchial tubes of the airways, meaning that air can pass more freely into and out of the lungs.
People with COPD often rely on inhalers to reduce their symptoms, but the effects of inhalers are short-lived and tend to only last for 24 hours. The dNerva targeted lung denervation system helps to combat this, providing a procedure which, in most cases for patients who are suitable, should be a one-off treatment and require no re-treatment later in life.
“We’re not saying this treatment is an answer to all things COPD-related for everyone, but it offers a further tool in our therapeutic armamentarium,” says Professor Shah. “Ultimately, we’re striving to improve the lives of individuals with COPD.”
Who is targeted lung denervation for?
Targeted lung denervation treatment is for patients with moderate to severe COPD, a high symptom burden and a history of COPD exacerbations or lung attacks.
“For patients with severe airflow limitation, who are not responding well to maximal medical therapy, this treatment offers alternative means to try and improve their quality of life and reduce the frequency of their flares,” explains Professor Shah.
Treatment with the dNerva lung denervation system is suitable for patients aged 40-75 with a body mass index (BMI) of between 18-35. Further to this, they must have stopped smoking or vaping for at least two months prior to treatment, as this can exacerbate COPD symptoms.
Factors which could make a person unsuitable for treatment include having:
- active asthma
- ongoing gastrointestinal-related symptoms
- implanted electronic devices
Due to the radiofrequency that is delivered during Nuvaira®’s procedure, if a person has an implantable electronic device, such as a pacemaker, they are unsuitable for this treatment.
For more information or to book an appointment, please contact our customer care team.
Related content
-
Chronic obstructive pulmonary disease (COPD)
Chronic obstructive pulmonary disease is a group of conditions that affect your breathing and quality of life. Learn how to effectively manage your symptoms.
-
Lung health assessment
Our lung health assessment service is accessible to patients with a range of symptoms, including breathlessness, cough, chest pain, and wheezing.
-
RejuvenAir®: 30-minute chronic bronchitis treatment


