Fungal lung diseases are an increasing burden on our public health systems with growing numbers of at-risk patient groups, including those with asthma and impaired immune systems. Our specialists have multi-disciplinary expertise across diagnosis and treatment of all fungal lung diseases to ensure patients receive optimal care.
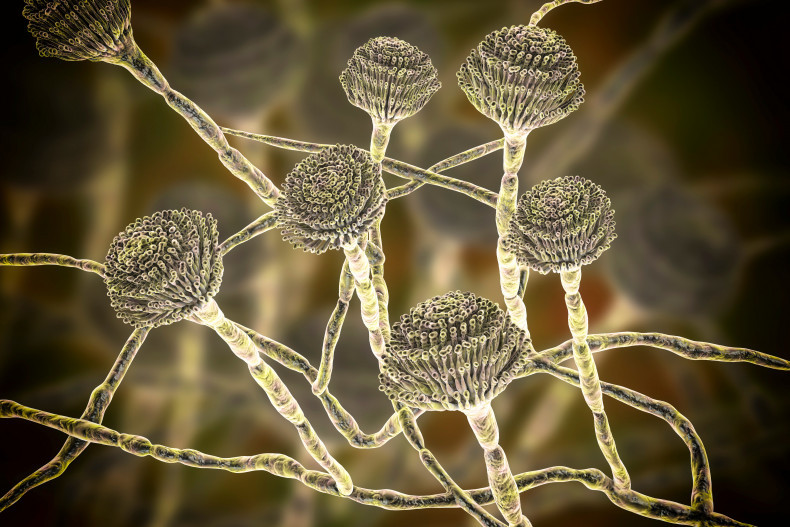
A 3D illustration of an Aspergillus fungus
Fungal lung disease: A growing burden
Fungi can cause lung disease through two mechanisms – by triggering an immunological reaction (e.g. asthma due to fungal sensitivity) or by direct infection of lung tissue.
Although fungal lung infections rarely occur in healthy people, they can result in life-threatening invasive disease in patients with an impaired immune system.
These include cancer patients undergoing chemotherapy, or those taking immunomodulating drugs for a solid organ transplant or autoimmune condition.
Underlying respiratory conditions can also increase the risk of chronic fungal infection and allergy such as COPD, asthma, bronchiectasis (including cystic fibrosis).
Unfortunately, the populations of these at-risk patient groups are growing, meaning that fungal lung diseases will place an increasing burden on public health systems.
Asthma and hypersensitivity to fungi
Sensitisation to fungi is associated with greater severity of asthma – it is estimated that up to 50% of adults with asthma referred to secondary care have fungal sensitisation.
This has led to the definition of a relatively new phenotype of asthma, called severe asthma with fungal sensitisation (SAFS). This condition is diagnosed as severe (poorly controlled) asthma in addition to a positive allergy test for fungal sensitisation.
Allergic bronchopulmonary aspergillosis (ABPA) is a rare and distinct condition to SAFS, affecting 1% of patients with asthma and 5-10% of those with cystic fibrosis (CF). Diagnosis is based on the worsening of underlying asthma or CF, with consistent radiology and positive allergy tests to Aspergillus spp.
Recent studies show a promising role of antifungals in treating SAFS and ABPA patients, with large improvements to quality of life reported in 60% of patients with SAFS.
“Uncontrolled fungal allergy or infection can lead to a great reduction in quality of life. It is therefore important to rule out pulmonary hypersensitivity to fungi and presence of fungal infection in patients with lung disease to ensure we develop the best treatment plan for them,” explains our consultant respiratory physician, Dr Anand Shah.

Sensitisation to fungi is associated with greater severity of asthma
Aspergillosis: The most common fungal lung infection
Aspergillosis can present in different forms depending on the underlying health of the patient and comorbidities.
Chronic pulmonary aspergillosis is characterised by cavitation and usually affects patients with underlying pulmonary conditions such as COPD, or those with common immunosuppressive conditions like diabetes.
The disease usually presents with a prolonged and relapsing cough, dyspnoea, and weight loss. Acute symptoms may include haemoptysis and pulmonary haemorrhage, particularly if an aspergilloma is present. Due the relapsing nature of the condition, it can be challenging to treat.
In addition to its association with chronic pulmonary aspergillosis, an aspergilloma can develop in the lungs following a cavity caused by previous infection with TB, pulmonary sarcoidosis, COPD or other lung disease causing cavitation.
Haemoptysis can be present in up to 60% of patients with an aspergilloma and be life-threatening. Presentation with cough and fever is not frequently observed and patients may be asymptomatic, with diagnosis confirmed incidentally with a chest X-ray. Lung resection may need to be considered if patients become symptomatic and antifungal therapy does not work.
Invasive aspergillosis is a disseminated form of the infection affecting significantly immunocompromised patients – for example, it affects an estimated 10-20% of patients after a bone marrow transplant.
Although it often starts in the lung, it can involve any other organ and/or tissue through haematogenous spread, including the brain. Due to this, it has a high mortality rate of 30-95%.
“Invasive aspergillosis can be a difficult condition to diagnose, and symptoms can include fever, cough, and shortness of breath. If it is suspected, a CT assessment with a specialist cardiothoracic radiologist is likely to be needed to spot the subtle indicators in the lungs,” explains our infectious diseases physician, Professor Darius Armstrong-James.

Young patients with cystic fibrosis are at risk of aspergillosis
Monitoring antifungal resistance
The only oral antifungal treatments active against Aspergillus species are the triazole group (which include voriconazole and itraconazole) and are used as first-line therapies.
Unfortunately, resistance to azole antifungal drugs is growing and it is estimated that up to 19% of Aspergillus infections are azole resistant.
Antifungal resistance is driven in two main ways. The first way it can arise is in patients with chronic aspergillosis where the infection spontaneously acquires resistance with prolonged use of azole drugs.
The second driver is agriculture and the widespread use of azole-based pesticides that are similar to triazole drugs. Genetic testing has determined that patients can be infected with azole-resistant Aspergillus strains from the environment which have acquired resistance in this way.
Antifungal resistance greatly influences patient outcomes. A recent cohort study showed that mortality in patients with voriconazole-resistant invasive aspergillosis was 20-30% higher than with voriconazole-susceptible disease.
Although slightly less effective, alternative treatments for pan-azole resistant infections are available, including intravenous amphotericin B.
“Drug sensitivity testing and ongoing therapeutic drug monitoring are an important part of treating aspergillosis to identify resistance as soon as possible and ensure the best outcomes – particularly in those receiving long-term antifungal therapy,” explains Dr Shah.
Multi-disciplinary expertise needed for accurate diagnosis and monitoring
“Royal Brompton and Harefield hospitals is the largest centre for fungal lung diseases in south England and we see over 600 patients a year. Our multi-disciplinary expertise enables us to quickly and accurately diagnose these conditions which can otherwise be challenging and require specialist diagnostic tools,” explains Dr Shah.
Professor Armstrong-James adds: “Our interventional radiology consultants can help discern even the most subtle signs of fungal lung disease and work alongside our expert histopathologists to detect pathogens not often observed at other centres.”
“Our combined expertise enables us to detect antifungal resistance at the earliest stages to deliver an optimal treatment plan tailored to each patient. We also have some of the world’s leading cardiothoracic surgeons should surgery be required, as may be the case for an aspergilloma.”
Dr Shah is an expert in fungal lung disease, as well as respiratory infection including bronchiectasis, cystic fibrosis and general respiratory diseases. Professor Armstrong-James’ expertise extends to all types of fungal infections, as well as viral, bacterial and parasitic infections. He also leads the diagnostic fungal service at Royal Brompton Hospital, with highly specialised services and tests for diagnosis of fungal lung infection.
Dr Shah and Professor Armstrong-James are both key academic researchers in fungal lung disease, with a broad portfolio of basic and clinical research through both Imperial College London and King’s College London.
Contact us
To find out more about our expertise in fungal lung diseases or to refer a patient, please contact our team.