The choice of aortic valve replacement procedure in young and middle-aged adult patients is challenging. It needs to provide durable haemodynamic properties that enable an active lifestyle desired by this age group, while avoiding valve-related reoperation for as long as possible to maintain an excellent quality of life.
Mechanical valves are very durable and most frequently implanted in this age group but require lifelong anticoagulation that exposes patients to haemorrhagic and thromboembolic complications. A biological valve is the most suitable for younger patients, particularly under 30, as they do not require anticoagulation. However, both bioprosthetic valves from animals and aortic valve homografts deteriorate at a high rate and require reoperation within a few years.
Trials have demonstrated favourable results for the Ross procedure in delivering a durable biological valve replacement with haemodynamic properties that are ideal for this patient population without the need for anticoagulation and our experts are currently trialling it in combination with the PEARS procedure to increase its durability even further.
Aortic valve replacement in younger patients
Aortic valve replacement is the most common form of heart valve surgery. It is used to correct aortic valve disease, the most common of which are aortic stenosis and aortic regurgitation. Although age is a risk factor for both these conditions, they can be congenital in nature and so affect younger patients.
Replacement options include mechanical valves, bioprosthetic valves, aortic valve homografts and the Ross procedure. However, there is currently no clear guidance on the best option and the choice of aortic valve replacement has important implications for long-term outcomes.
In older patients over 60, the choice of aortic valve replacement is straightforward, as there is no survival advantage between bioprosthetic or mechanical valve at this age. However, in young and middle-aged adult patients that require aortic valve replacement, the choice is more challenging.
Due to a longer life expectancy, these younger patients are exposed to higher cumulative risks of valve-related complications. They are also more likely to want to pursue higher levels of physical activity after an operation than older patients and, for women of childbearing age, may be contemplating pregnancy.
An ideal aortic valve replacement for young and middle-aged adult patients will therefore need to minimise valve-related complications and provide durable haemodynamic properties that allow patients to lead an active lifestyle with an excellent quality of life.
Mechanical valves are the most frequently implanted in young and middle-aged adult patients primarily due to the ease with which they can be implanted and their durability. However, as they are thrombogenic, they require lifelong anticoagulation and expose patients to a continuous hazard of haemorrhagic and thromboembolic complications.
The management of anticoagulants can be particularly problematic during pregnancy, where they can pose a significant risk to both mother and foetus. The risk of thromboembolic events with mechanical valves is also significantly increased with pregnancy. Biological valves are the most suitable for younger patients, particularly those under 30, as they do not require anticoagulation. However, both bioprosthetic valves and aortic valve homografts are associated with predictable higher rates of valve deterioration and need for reoperation when implanted in young adults. Bioprosthetic valves also have the potential for accelerated degeneration with pregnancy.
The Ross procedure may offer an alternative, more favourable option for biological aortic valve replacement in young and middle-aged adults.
The Ross procedure: A favourable approach for younger adult patients
The Ross procedure utilises the anatomic similarity between the aortic and pulmonary valves. The diseased aortic valve is first removed and replaced with the patient’s own healthy pulmonary valve as an autograft. The patient’s pulmonary valve is then replaced with a cryopreserved donor valve as a homograft.
The pulmonary valve autograft undergoes adaptive remodelling enabling it to mimic the function and highly sophisticated anatomy of the native aortic root. This translates to better long-term clinical outcomes than all other aortic valve substitutes, including aortic valve homografts which become acellular a few weeks after implantation.
Studies have shown that haemodynamic performance in patients undergoing the Ross procedure closely mirrors that of native aortic valves in healthy individuals during maximal exercise performance. As human valves are used, patients also do not require anticoagulation. Due to both factors, patients experience an enhanced quality of life when compared to mechanical aortic valve replacement.
A recent long-term study of the outcomes of the Ross procedure on 414 patients over 18 years demonstrated an excellent long-term survival rate of 89.3% at 15 years, which was similar to a normal age- and sex-matched population. There was also a low incidence of reoperations.
A separate study compared the cost-effectiveness of the Ross procedure with bioprosthetic and mechanical valves in young and middle-aged adults. It demonstrated that the Ross procedure was more economically efficient in the longer term with a lifetime incremental net monetary benefit of £60,952.
Due to the complexity of the Ross procedure, it is most safely performed at experienced, high volume centres where operative mortality is comparable to that of conventional prosthetic aortic valve replacements. Our specialist hospitals have been performing the Ross procedure for over 30 years with favourable results.
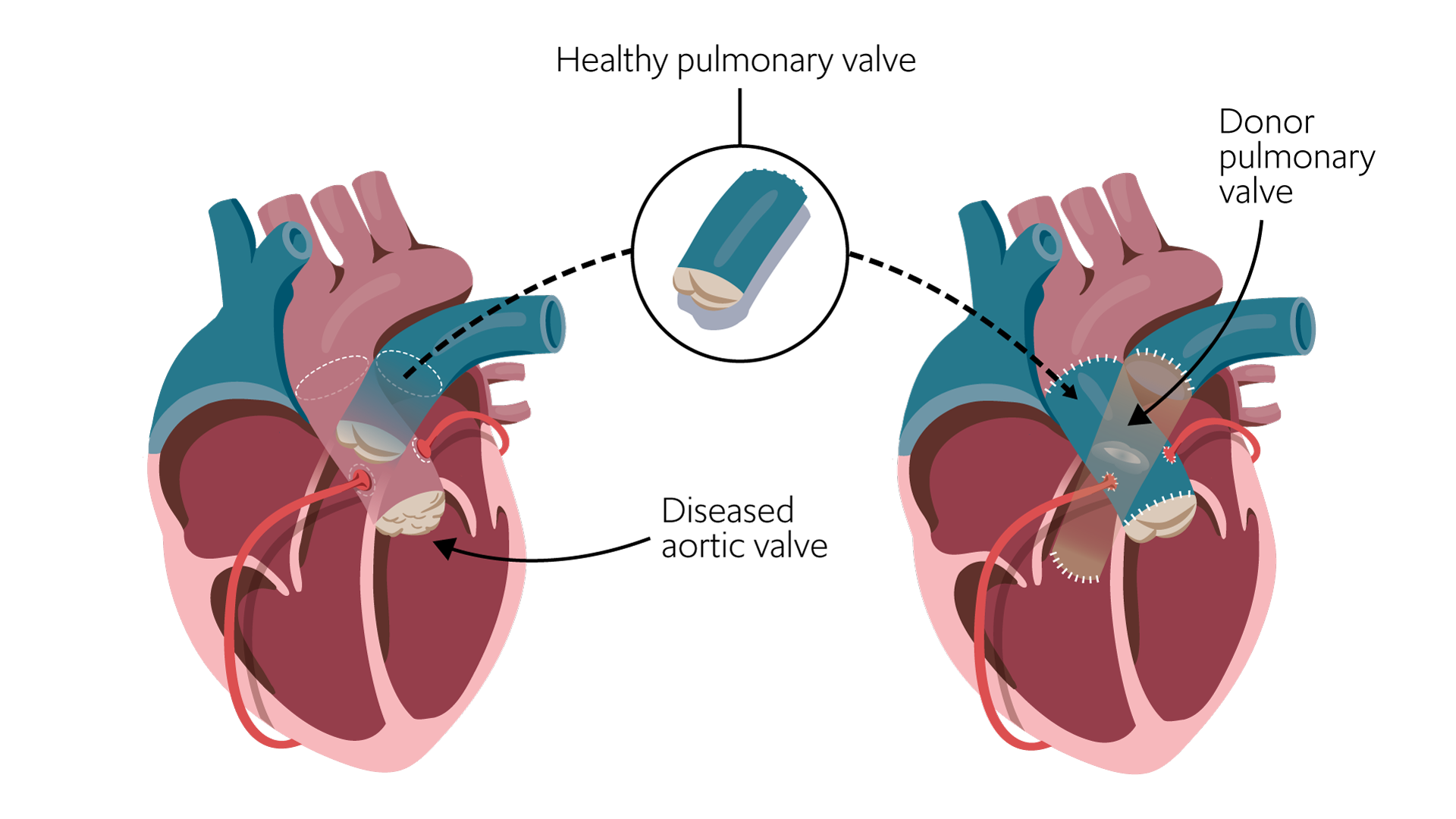
The Ross procedure: The diseased aortic valve is removed and replaced with the patient’s own healthy pulmonary valve - the pulmonary valve autograft. The patient’s pulmonary valve is replaced with a cryopreserved donor pulmonary valve.
Enhancing the ross procedure with PEARS
Although excellent long-term results have been demonstrated with the Ross procedure, the pulmonary valve autograft can require reoperation 15 years later in approximately 10% of patients. This may occur due to progressive aortic root dilation or anatomic mismatch between the original diseased aortic valve and pulmonary valve autograft, which can lead to damage over time.
Aortic root reinforcement during the Ross procedure has been trialled and has shown to reduce the need for reoperation for pulmonary valve autograft failure. Aortic root reinforcement may therefore be performed prophylactically to prevent aortic dilation or therapeutically to correct anatomical mismatch.
Personalised external aortic root support (PEARS) is a relatively new aortic root reinforcement system. Originally developed at our hospitals for patients with Marfan syndrome – where patients experience aortic dilation at a young age, a synthetic ExoVasc polymer mesh sleeve is used to support the aorta and prevent it from expanding.
The ExoVasc mesh support utilises advanced medical imaging and computer-assisted 3D printing to create a precise model of the patient’s aorta and aortic valve that is personalised to the unique anatomy of the patient. This model is then used to form the textile ExoVasc implant. The ExoVasc textile implant created has 0.7mm pores which enable the patient’s cells to enter and adhere it firmly to the patient’s tissues for greater long-term durability.
A recent multi-centre, prospective cohort study on 117 patients receiving the PEARS procedure for a dilated aortic root (without the Ross procedure) demonstrated a low risk of death and requirement for re-operation after a minimum of one-year follow-up.
“The PEARS procedure has been successfully performed on over four hundred patients with Marfan syndrome worldwide. However, its use in the Ross operation is fairly new,” explains our consultant cardiac surgeon, Professor John Pepper, who pioneered the PEARS procedure at Royal Brompton Hospital and advises our consultants on this and the Ross procedure.
“By adding aortic root reinforcement with PEARS to the Ross procedure, we hope to reduce the number of patients requiring reoperation on the pulmonary valve autograft. For young and middle-aged adult patients, we want to make sure that any treatment offered enables them to live for as many years without re-intervention as possible, with an excellent quality of life.”
In the Ross-PEARS procedure, it is the pulmonary valve autograft that is modelled and an ExoVasc implant produced to support it when it is re-implanted to replace the aortic valve.
Our consultants are leading experts in the combined Ross-PEARS procedure, with over 40 procedures performed so far across our hospitals and our consultant cardiac surgeons, Mr Jullien Gaer, Mr J Andreas Hoschtitzky, Mr Mario Petrou and Professor Darryl Shore all perform it at our centre.
Mr Conal Austin, consultant cardiothoracic surgeon at Guy’s and St Thomas’ NHS Foundation Trust – which we have recently merged with, also performs the Ross, PEARS and combined Ross-PEARS procedure, but does not currently operate at Royal Brompton and Harefield hospitals.
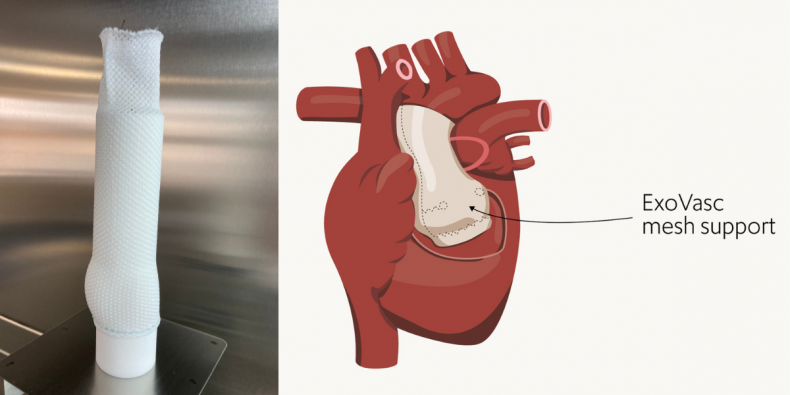
The PEARS procedure: (L) the ExoVasc mesh support formed on an anatomically precise model of the patient’s aorta and (R) a visual of the mesh support in situ implanted around the patient’s aortic root.
Helping Fabio get active again
Fabio was used to keeping a close eye on his heart from a young age. This is because he was born with a ventricular septal defect.
To resolve his heart problem, doctors in Italy (where he was born) performed corrective heart surgery at the age of 15.
“My doctors managed to fix my heart and I lived a relatively normal life with routine heart checks,” says Fabio.
“I worked for many years in the cruise industry which was physically demanding, but I enjoyed staying active and got to see the world.”
In 2014, he moved to the UK where he was referred to the care of our consultants at Royal Brompton Hospital to continue his routine heart checks and remained fit and healthy.
Encouraged by his partner, he took up Tai Chi and yoga, which he practiced for over five years. He explains: “When you’re born with a heart condition, you become very conscious of your health and I have always tried to stay fit and healthy.”
However, in 2019 at the age of 39, he noticed his heart health start to deteriorate gradually.
“I started to experience heart palpitations and feeling faint and dizzy. At first, this happened once every couple of months, but this became multiple times a week,” Fabio explains.
Unfortunately, his symptoms caused him to stop driving, cycling, and taking part in the activities he loved.
Our consultants assessed Fabio’s heart and found his aortic valve was faulty, causing him to experience the symptoms he felt. This is when he was referred to the care of Mr Hoschtitzky for assessment for the Ross-PEARS procedure to replace his aortic valve.
“Mr Hoschtitzky talked me through my treatment options and the Ross-PEARS procedure was a no brainer. I didn’t want to be on blood thinners for the rest of my life and I would get to keep my own heart valve,” he says.
In October 2020, Mr Hoschtitzky successfully performed the Ross-PEARS procedure on Fabio, and he is now on a steady path to recovery – he has even started jogging again.
“It’s crazy to think that I was on a surgical bed and feeling really unwell two months ago and now I’m jogging. I know I still have a journey ahead in my recovery and getting back into the more intense sports I enjoyed but it’s going great so far,” he explains.
“I only have extremely nice words for everyone at Royal Brompton Hospital – from the nurses to the consultants. They looked after me really well and I feel very fortunate to have had a procedure that isn’t widely available.”

Fabio was used to keeping a close eye on his heart from a young age. This is because he was born with a ventricular septal defect.
Related content
-
Aortic disease
Aortic stenosis is a narrowing of the aortic valve opening, restricting blood flow to the aorta.
-
Personalised external aortic root support (PEARS)
Personalised external aortic root support treats and manages aortic dilation and dissection in patients with Marfan syndrome.
-
Valve repair or replacement
Heart valve surgery can repair or replace a damaged valve.


