What is an aortic valve
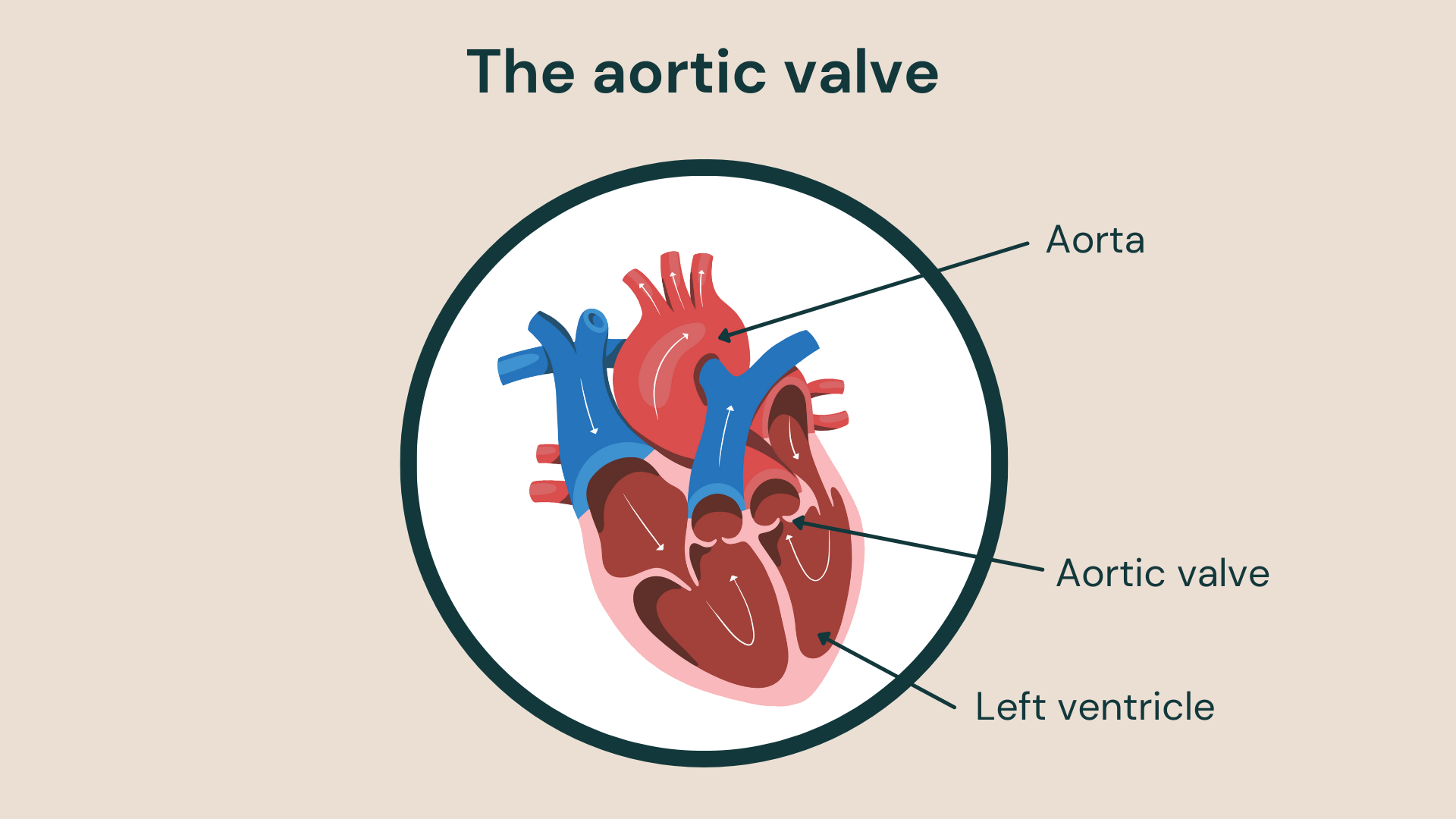
The aortic valve is one of four valves in the heart – alongside the tricuspid valve, pulmonary valve and mitral valve – that controls blood flow. It connects the left side of your heart with your aorta (the main artery that carries blood away from the heart). The aortic valve regulates the flow of blood through the aorta and keep blood from congesting the heart.
If the aortic valve begins to not function properly, then you may have aortic valve disease. This can occur when the valve may be stiff (otherwise known as aortic stenosis), or if blood is flowing back to the heart because the valve is not closing properly. If this happens, then you may need an aortic valve replacement.
Surgical aortic valve replacement (SAVR)
Surgical aortic valve replacement (SAVR) can treat a faulty aortic valve, reduce unpleasant symptoms and improve your quality of life. It’s the gold standard treatment for aortic stenosis, but deciding whether to have open heart surgery can be difficult.
Your cardiothoracic surgeon and cardiologist will be the best source of information and advice about the pros and cons of aortic valve replacement surgery in your case. However, this blog provides background information about the success rate of aortic valve replacement.
We will discuss the success rate of aortic valve replacement surgery and explore studies looking at surgical results. We’ll also look at the potential risks and complications of SAVR. Finally, we’ll explore the success rate of transcatheter aortic valve implantation so that you can make an informed choice about your medical care.
The success rate of aortic valve replacement surgery
A long-term National Institute of Health Research (NIHR) review into the surgical replacement of aortic valves showed that these procedures offer good long-term survival.
The study examined data from more than 90 studies observing long-term outcomes for people having SAVR with a biological valve made from animal tissue.
The study showed that people with aortic stenosis who had surgery to replace a narrowed valve have only a slightly reduced life expectancy than people without the condition. Post-operative survival ranged from an average of 16 years in people aged 65 or less, to between six and seven years for people over 75.
The 2017 review found that aortic valve replacement surgery had an overall mortality of 2%, which the NHS website says ‘is far lower than the risk associated with leaving severe aortic disease untreated’ and stroke risk of 3% or less.
How long do biological valves last?
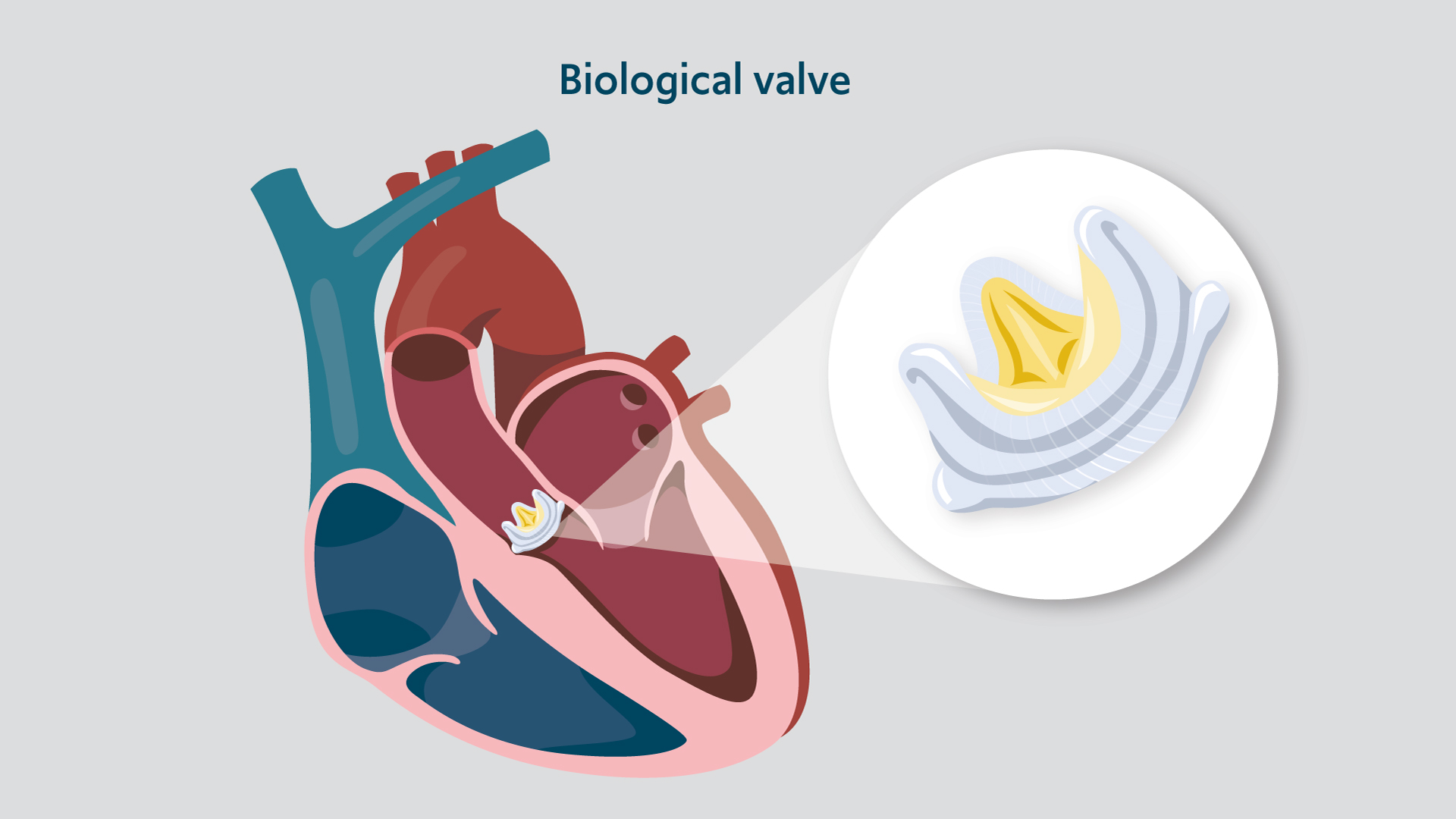
“Biological or bioprosthetic valves are made of animal tissue, either porcine from a pig or bovine from a cow. They wear out more quickly than mechanical valves, making them better suited to older people. However, they have benefits over mechanical valves in that they have a reduced risk of blood clots or blocked veins (thrombosis), which means that long-term blood thinners (anticoagulants) aren’t usually necessary” explains our consultant cardiac surgeon Mr Shahzad Raja.
In the NIHR study, bioprosthetic valves appeared safe, and they were linked to average lifespans when matched to the population having surgery. Ten years after replacement, the great majority of people (94%) had a functioning valve. After 20 years, more valves had failed, with 48% of valves deteriorating. The NIHR said:
“This large review indicates that bioprosthetic valve replacement for severe aortic stenosis is safe and gives survival outcomes comparable to the general population without aortic stenosis.”
“The long-term deterioration of the valves suggests a need for regular monitoring to identify people who may require a further valve replacement, especially after ten years” explains Mr Raja.
So, if you choose a bioprosthetic valve, you may need echo monitoring and possibly a replacement valve after ten years or so.
Risks of aortic valve replacement surgery
There are risks involved with any surgery. Serious problems are uncommon with SAVR – but it is major open-heart surgery. Your cardiothoracic team will work to reduce any complications and support your healthy recovery.
“The risk of complications with aortic valve replacement surgery depends on your general health and the health of your heart. People who are frail, elderly, or have multiple underlying conditions may be more vulnerable to problems,” explains Mr Raja.
Talk to your hospital team about the risks and benefits in your case. This is a summary of the main risks:
- Infections: You could develop an infection in the wound, lungs, bladder or the new valve. The team will give you antibiotics to reduce your infection risk
- Bleeding
- Thrombosis (blood clots): Clots can develop, particularly in mechanical valve replacement. You will need to take anticoagulants for life to prevent blood clots if you are at risk
- Stroke
- The valve may wear out over time, with bioprosthetic valves typically lasting for a shorter time
- Cardiac arrhythmia: One in four people develop an abnormal heart rhythm after aortic valve replacement. This usually settles, but up to one in 50 people will need a pacemaker to regulate their heartbeat
- Kidney problems: In the days after surgery, your kidneys may need support to function, and some people need temporary dialysis – a procedure used to remove waste products and excess fluid from the blood
- Sadly, in around 2% of people, aortic valve replacement surgery complications can be fatal. However, this is lower than the risks of not treating severe aortic valve disease. Over 50% of people with advanced aortic valve disease will likely die within 5 years without treatment.
Success rate of TAVI
TAVI, sometimes referred to as TAVR, is a minimally invasive procedure used to treat aortic valve disease. This technique involves inserting a catheter into your leg or upper chest and passing it to your aortic valve. The catheter then helps to guide a replacement valve to your aortic valve to be placed over the old, damaged one. The new valve then replaces the old valve leaflets and tissue, and takes over blood flow regulation.
Compare to SAVR, TAVI is regarded as a safer procedure because it doesn’t involve open heart surgery. Therefore, it is considered a viable alternative for elderly patients who are unsuitable for SAVR. A Dutch research study in 2020 found that transcatheter aortic valve implantation (TAVI) offers outcomes that are comparable to surgical aortic valve replacement surgery in older people. In patients that are over 80, their survival and quality of life after TAVI is similar to that in the matched general population. A 2020 review of the best research evidence showed that TAVI might reduce mortality from all causes at 30-days and after 1 year compared with SAVR.
Whilst TAVI may seem like a better option, there are many factors to consider. The viability of this procedure depends on the severity of the patient’s condition and the anatomy of their heart. For example, some patients will not be eligible for TAVI if their valves are too small or too large. Furthermore, due to the durability of the stent used in SAVR, a valve can last for up to 15 years. Whereas, a TAVI valve has an uncertain lifespan.
Currently, the National Institute for Health and Care Excellence (NICE) only recommends TAVI for people unsuitable for surgical aortic valve replacement due to age, illness or frailty. They are currently reviewing the guidance (as announced in November 2021), saying:
‘NHS England and Improvement are aware that transcatheter aortic valve implantation (TAVI) is clinically effective but not currently cost-effective for patients defined as intermediate or low risk for cardiac surgery for aortic valve disease.’
They added that:
‘TAVI may also have other benefits. It may be performed in a catheterisation laboratory without general anaesthetic, rather than an operating theatre. TAVI is also associated with a lower average length of overall hospital stay (around 3 days) compared with surgery (around 10 days)’.
Related content
-
Aortic disease
Aortic stenosis is a narrowing of the aortic valve opening, restricting blood flow to the aorta.
-
Aortic stenosis
Aortic stenosis is a disease that affects the main outlet valve of the heart and is the third most common cardiovascular disease.
-
Valve repair or replacement
Heart valve surgery can repair or replace a damaged valve.
-
Transcatheter aortic valve implantation (TAVI)
TAVI is a minimally invasive procedure where a new aortic valve is inserted into your heart.

